
There is no pain experienced when one is suffering from retinal detachment but warning signs appear much in advance. These include
Photopsia – experiencing sudden but brief flashes of light in the peripheral field of vision. These flashes more commonly occur when the eye moves
If you notice any of the above symptoms, schedule an eye check-up immediately.
Retinal detachment can occur as a result of
Rhegmatogenous retinal detachment– a break, tear or hole develops in the retina, allowing liquid to pass from the vitreous space into the sub retinal space between the sensory retina and the retinal pigment epithelium (the pigmented cell layer just outside the neurosensory retina).
Secondary or Exudative or Serous retinal detachment– an inflammation, vascular abnormalities or tumour causes fluid to build up under the retina (there is no hole, break or tear in this case), resulting in retinal detachment.
Tractional retinal detachment– an injury, inflammation or neovascularisation causes the fibro vascular tissue to pull the sensory retina from the retinal pigment epithelium. eg: Diabetic tractional retinal detachment.
You’re more likely to get a detached retina if you
Note: Retinal tears and retinal detachment are different things. Retinal tears often happen first. If these tears are not treated in time, fluids from within the eye may pass through the tear and separate the retina from its underlying tissue, causing retinal detachment. Retinal detachment may also happen without any warning. But this is more likely in the elderly or those suffering from extreme cases of myopia.
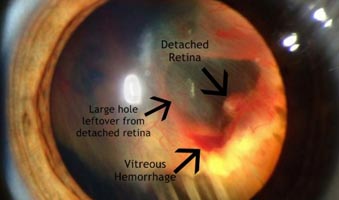
To diagnose retinal detachment, your ophthalmologist would examine the insides of your eyes using an ophthalmoscope. It provides a highly detailed 3-D view, allowing the doctor to see any retinal holes, tears or detachments. Ultrasonography may also be performed which uses sound waves to create the picture of your eye on a video monitor.
To re-attach the retina and prevent future occurrences of retinal detachment, eye surgery needs to be performed. Different modes of treatment include
Copyright © 1987-2024 Ojas Eye Hospital All rights reserved | Privacy Policy
*Disclaimer: All information on www.lasikindia.com for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider.