
Dr. Niteen Dedhia’s talk on Keratoconus
Early cases of Keratoconus are diagnosed many a times on routine eye examination by the eye practitioner. Keratoconus causes myopia or nearsightedness and irregular astigmatism. The patients experience frequent changes in power of glasses with fluctuation in vision. Some patients also have glare and sensitivity to light especially during night.
In advanced stage of Keratoconus, even corrective prescription glasses does not help the patient to see clearly and they have to switch to using hard or semi-soft contact lenses.
Your eye care practitioner can diagnose early stage of keratoconus after a detailed eye examination including retinoscopy, slit lamp examination and sophisticated tests like topography to check the shape and curvature of cornea and pachymetry to determine the thickness of the cornea.
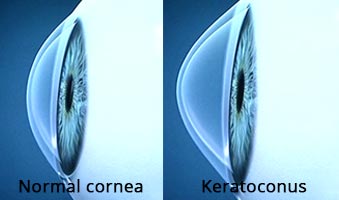
The exact cause of keratoconus is not known but latest research suggests that the cornea becomes weakened due to imbalance of enzymes within the corneal tissue leading to thinning and bulging of cornea.
 Image as seen by the normal eye
kat-after
Image as seen by the normal eye
kat-after  Same image as seen by a keratoconus patient
Same image as seen by a keratoconus patient
Keratoconus also shows some genetic predisposition. It may transmit from parent to children and affect more than one family member. It is also associated with excessive eye rubbing as it is more common in allergic conjunctivitis patients who have itching and tend to rub their eyes very often. Other risk factors are overexposure to ultra violet rays, chronic eye irritation and improperly fitted contact lenses.
In early stages, when the cornea is still regular, corrective prescription glasses or soft contact lenses can help the patients. As keratoconus advances the corneal surface becomes increasingly irregular and these options do not help adequately.
In intermediate stage, there are various treatment options including different type of contact lenses:
Rigid Gas Permeable contact lenses– They are the first choice of treatment when glasses fail to help the patient. They provide a smooth refractive surface replacing the irregular cone like surface of the cornea, thus enabling the patient to see clearly.
Lens fitting in keratoconus can be a demanding and time consuming process. It requires frequent visits to the eye doctor to get a perfect and comfortable fit. Rigid Gas Permeable lenses (RGP) however may not be as comfortable as soft contact lenses.
“Piggybacking” Contact Lenses– Some eye doctors practice “piggybacking” where a soft contact lens is first placed on cornea to give it a cushion like effect and over it RGP lens is fitted. Thus, it combines the best features of both lenses in the sense that it makes the wearer comfortable and at the same time gives crisp vision. The fitting should be perfect to ensure good oxygen permeability to the cornea as the patient will be wearing two lenses. However, with newer high oxygen permeable lenses this is not a problem.
Hybrid Contact lenses– Some manufacturers have come up with this unique design of contact lenses where the central visual portion is made up of high oxygen permeable rigid material and peripheral anchoring portion is of soft hydrogel material. This also maximizes the best feature of both lenses and improves wearers comfort as well as visual performance in keratoconic eyes with a single contact lens.
In the last decade, with newer technological advances in treatment modalities for keratoconus, INTACS and C3-R have showed promising & encouraging results.
INTACS Intacs are plastic insertable devices approved by FDA in 2004 for treatment of keratoconus and myopia of upto 3 dioptres. These semicircular rings of various thickness and diameters are placed within the middle layers of the cornea. Their placement remodels and reinforces the cornea, eliminating all or some of its irregularity caused by keratoconus. At the same time it flattens the cornea, correcting the myopic & astigmatic refractive error to a considerable extent.
Intacs placement is a simple procedure and does not require any tissue removal. They are reversible and cannot be felt by the patient after insertion and healing. They require no maintenance. However, glasses or contact lenses may be required even after successful intacs implantation. They have been shown to improve vision, thereby saving the patient from requiring corneal transplantation.
C3-R Treatment ( Corneal Collagen Cross Linkage with Riboflavin) It is a non-invasive and very popular procedure for treatment of keratoconus. It strengthens the collagen tissue which forms the fabric of cornea. This is simple 60 minutes in-office procedure. Eye drops containing Riboflavin (Vitamin B2) are put on the cornea and then activated by Ultra-violet light(UV-A). This increases the collagen cross linking causing strengthening of cornea thereby stopping it from bulging outwards and arresting keratoconus from progression.
In the 3 years results of clinical study in human eyes, C3-R treatment has shown arrest of keratoconus progression in all treated patients. C3-R procedure changes intrusive bio-chemical properties of the cornea increasing its strength by almost 300%. It is the only procedure currently available to halt the progression of the disease.
Penetrating Keratoplasty It is the last option when all the above methods fail to restore optimum useful vision to the patients. In this procedure, the cornea which forms the transparent outer covering of the eye is replaced by a donor cornea. It is an intra ocular surgery and requires long term healing and consistent follow-up. Even after a successful transplant, glasses or contact lenses may be required to give useful clear vision.
Another viable option for management of keratoconus is DALK (deep anterior lamellar keratoplasty). In contrast to the previous type of corneal transplant, in this procedure only the outer laters of the cornea are replaced. It is an extra-ocular procedure with lesser complication rates and provides earlier visual rehabilitation for the patient.
Copyright © 1987-2024 Ojas Eye Hospital All rights reserved | Privacy Policy
*Disclaimer: All information on www.lasikindia.com for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider.